These AI-Powered Nonprofits Are Making Healthcare More Equitable and Effective

Originally published in Stanford Social Innovation Review by Kevin Barenblat and Nick Cain.
After her third child was born prematurely, Ruth, a 25-year-old Kenyan mother, didn’t know where to turn. “When the doctor approved that we could go home, I felt afraid since this birth was different from the first two births,” she said.
Thankfully, months before, Ruth had signed up for PROMPTS, an AI-powered digital health navigator where she could ask questions, get help, and assuage concerns, all over SMS.
“PROMPTS has been my guiding light. Whenever I faced a difficulty, I quickly relied on the messages to help navigate it,” she said. When her baby caught an eye infection, PROMPTS asked a series of questions and recommended she seek medical care for her son, who received the care he needed.
AI has enabled PROMPTS to dramatically expand its reach—Ruth is one of 2.4 million African women who rely on it—and to triage the 7,000 messages it receives every day. A platform of the nonprofit Jacaranda Health, PROMPTS (more on this below) is one example of how AI-powered nonprofits (APNs) are at the vanguard of using AI to improve access to and quality of health care.
In our review of how healthcare APNs are using AI to advance health equity, we found a broad array of use cases: increasing access to quality healthcare, reducing mortality rates, discovering new medical treatments, and pioneering new forms of care.
In this article, we identify key themes from our research, highlight case studies of health-focused APNs, and make recommendations for healthcare nonprofits looking to adopt AI.
Major Themes: How Healthcare Nonprofits Leverage AI
Research from Fast Forward and analysis from the Patrick J. McGovern Foundation (PJMF) revealed four themes of how healthcare APNs leverage AI to advance health equity:
- AI unlocks the power of data. The healthcare industry generates 30 percent of the world’s data volume. The data is complex. Regulations abound. Ethical issues make privacy paramount. But nonprofits are using AI to make sense of this data and use it to inform decision-making around how to drive health equity.
- AI makes healthcare workers more effective. AI has become an indispensable partner for healthcare workers and providers. APNs are applying AI to turbocharge the ability of healthcare workers to reach more patients and deliver high-quality care. AI can make the best human-powered care even better and more scalable.
- AI puts more power in the hands of patients. The organizations we studied are giving patients more power to control their own health care. AI agents provide patients, especially those in remote locations, with personalized health advice, monitoring, and care.
- Nonprofits leveraging AI are tackling issues overlooked by for-profit companies. Nonprofits are leveraging AI in novel ways: from accelerating medical research for neglected diseases to building free, open-source software that puts medical information in the hands of those who need it most.
Underpinning these four themes is one common denominator: AI tools in the healthcare space need to be carefully trained and continuously evaluated to ensure AI upholds ethical standards and doesn’t reinforce existing inequities. Algorithmic biases can exacerbate existing inequities and lead to harmful outcomes (in one example, people of color were underrepresented in AI training data for skin cancer detection, leading to a heightened risk that skin cancer could go undetected). The nonprofits we studied centered equity and ethics in their deployment of AI.
For funders, the insights from this research provides a roadmap for future grantmaking. “There should not be a single funder in the world today who isn’t trying to figure out how AI can equip and support their nonprofits that they partner with and trying to understand how this is going to impact basic dignity and equity across the communities they say they support,” PJMF President Vilas Dhar told the audience at the Microsoft Global Nonprofits Leader Summit earlier this year.
Three Case Studies of Health APNs
Intelehealth
Intelehealth is an open-source telemedicine platform that connects patients and frontline health providers in rural communities throughout India with remote doctors to deliver affordable health care.
By 2030, the World Health Organization estimates a global shortage of 10 million health care workers. For every 10,000 people in rural communities across India, there are less than two doctors and four nurses.
With such limited access to care, rural communities incur prohibitive burdens when seeking medical help: hours of travel, expensive transit costs, and lost income due to days of work missed. When patients do access care, the quality is often substandard. The doctors and nurses who do serve remote communities often see hundreds of people per day. The result? People go without care and preventable diseases take lives.
Women suffer the most. In rural communities in India, 90 percent of women are not allowed to make independent decisions about their health care, and only 52 percent are allowed to go to a health facility alone.
Intelehealth’s open-source, free telemedicine platform improves healthcare access and quality. Powered by a novel digital assistant called Ayu, the telemedicine platform is both provider-to-provider (connecting frontline healthcare workers with doctors) and direct-to-patient (connecting doctors to patients for in-home consultations). The whole platform is interoperable with third-party diagnostic devices that capture vitals and conduct glucose monitoring.
Intelehealth is piloting how AI can help health workers manage a larger population efficiently. They are currently testing how AI-powered image analysis tools could drive early detection of diseases by analyzing medical images like photos, x-rays, and MRIs. The pilot includes how natural language processing (NLP) applications could help health care professionals extract pertinent information from medical documents, improving decision-making and enhancing the quality of care.
Intelehealth is piloting a range of commercially available AI tools (Google’s Gemini, OpenAI’s ChatGPT, and Meta’s Llama). To mitigate errors and hallucinations, Intelehealth regularly refines its prompts, re-trains its models on relevant cases, and provides datasets that enrich the algorithms’ understanding of regional and demographic variations.
Ayu is increasing access, improving quality, and advancing gender equity. To date, it has been deployed to over 100,000 healthcare workers throughout India in partnership with various state governments.
In our landscape analysis of APNs, it’s a prime example of AI as a navigator: AI to help a user through a complex process, guiding them through a personalized pathway.
Jacaranda Health
Jacaranda Health uses AI to improve the quality of care for new mothers and newborns across Sub-Saharan Africa. Its digital health platform, which responds to thousands of inbound questions every day, uses AI to send information and support to mothers via SMS.
Sub-Saharan Africa has the highest maternal mortality rate in the world. One contributor to maternal deaths is that mothers are not empowered or informed to seek care at the appropriate time. In Kenya, delays in seeking care lead to one-third of all maternal deaths. The good news is that timely information can help; Jacaranda finds that 91 percent of women would seek care if they were notified that they were in danger.
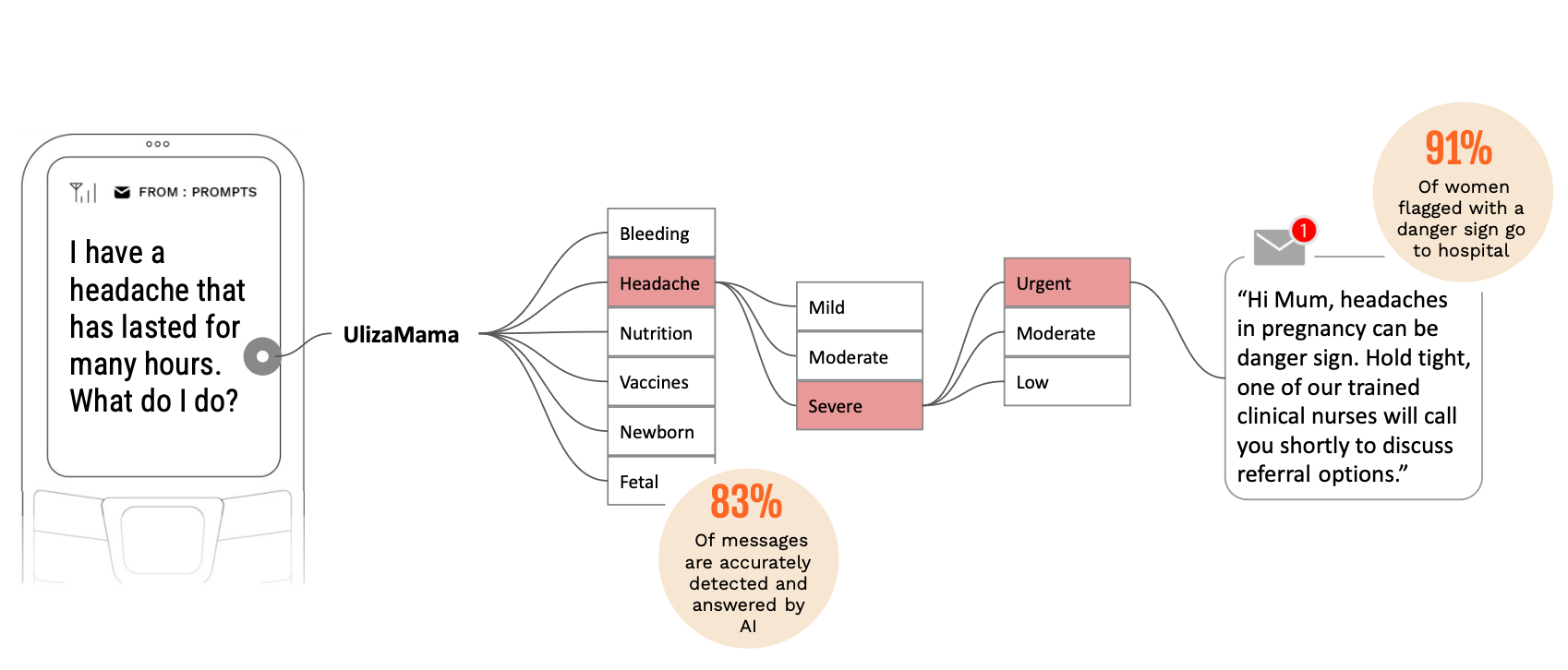
Jacaranda’s PROMPTS platform is a conversational, SMS-based health platform that provides personalized information to mothers throughout pregnancy and postpartum, and uses an AI-based clinical help desk to read, respond to, and triage incoming questions from mothers. It runs on a locally-customized LLM, called UlizaLlama, which is a first-of-its-kind LLM that operates in English and Swahili.
Trained on the 1.3 million questions that users have asked the platform, the model reads, responds to, and triages over 7,000 incoming messages every day from mothers—all in three languages. Jacaranda follows what’s become a best practice: having human agents review all AI-generated messages to ensure accuracy and edit for nuance.
With so many inbound messages, the LLM identifies potential danger signs and triages them according to urgency. For example, high-risk messages like bleeding during pregnancy are triaged in minutes to a team of agents who then call the mother and assess the best referral options (whether to a facility or local counseling service).
Before introducing UlizaLlama, Jacaranda’s PROMPTs platform was a human-to-human SMS chatbot between Jacaranda staff and mothers. But the demand quickly became unmanageable. With AI, Jacaranda can reach more mothers with life-saving information at a fraction of the price. The operating costs of PROMPTS is only US $0.74 per mother.
To date, over 2.9 million women have been enrolled on the platform. Of those, 81 percent of pregnant PROMPTS users attend more than four antenatal care visits, and 85 percent of mothers flagged for referral to a facility end up seeking care in a hospital.
In our landscape analysis of APNs, it’s a prime example of AI as a coach: dynamic AI that emulates human interaction and provides domain expertise.
Reboot Rx
Reboot Rx fast-tracks the discovery of affordable generic drugs that can treat specific types of cancer. It uses AI to scan hundreds of thousands of published medical research studies to identify the most promising low-cost generic drugs to repurpose for cancer treatment.
Worldwide, there are 20 million new cancer diagnoses every year, leading to 10 million deaths and $1 trillion in cancer-related costs. Depressing stats, but there is hope. Existing, low-cost, generic drugs developed for other health issues hold immense potential to treat specific types of cancer, but they need to be identified and repurposed.
Reboot Rx has found that 25 percent of non-cancer generic drugs have the potential to fight cancer, and the costs to repurpose an existing drug represent a mere fraction of the costs to develop a new one (less than $15 million to repurpose an existing generic drug, compared to more than $500 million to develop a new drug).
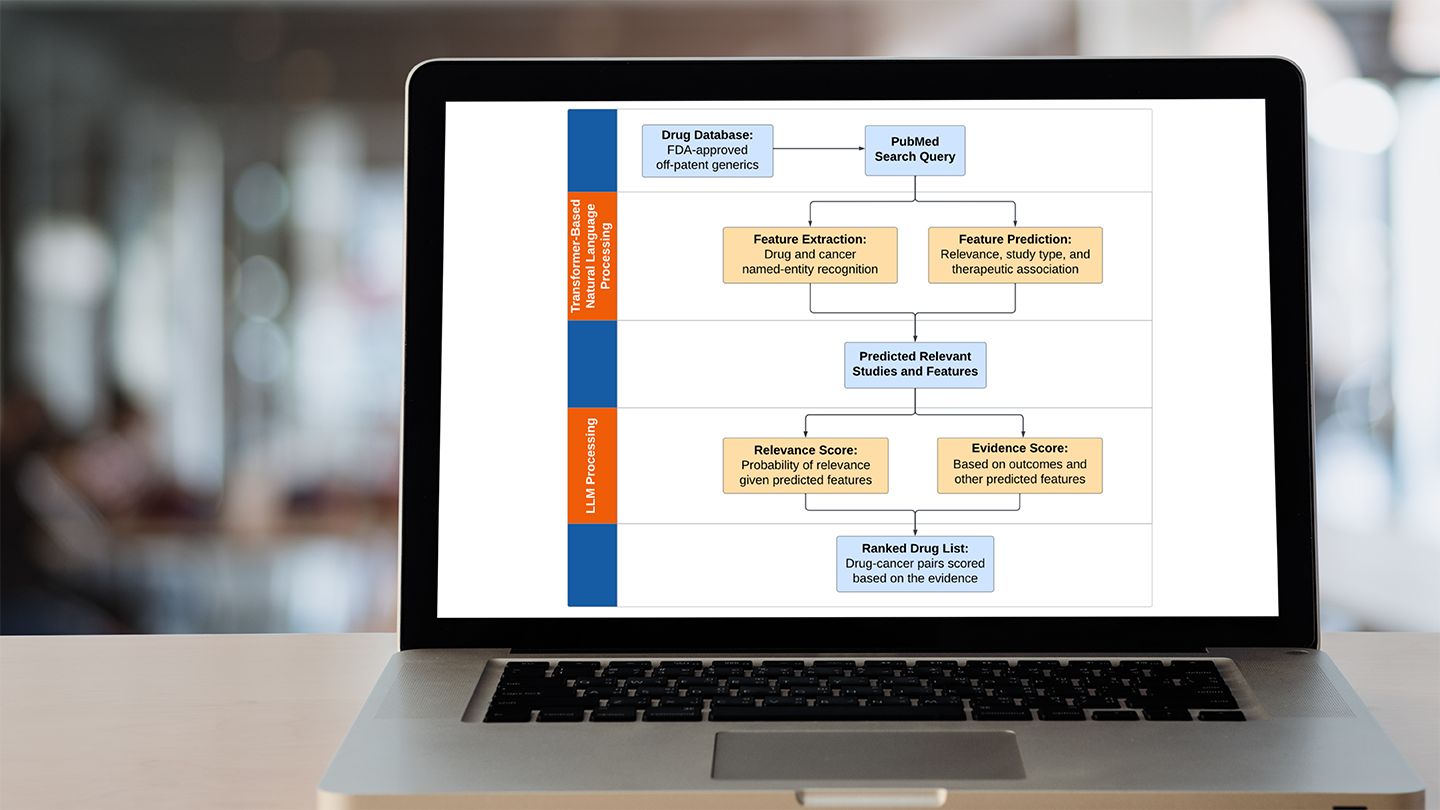
Reboot Rx uses a suite of AI tools—fine-tuned BERT models, biomedical information extraction models, and LLMs like ChatGPT—to review the global catalog of medical articles and pinpoint the most relevant studies. Then AI highlights pertinent information in the articles and ranks the drugs based on the totality of evidence.
The end result: the AI-driven approach significantly accelerates the drug development timeline by automating tasks. What used to take years now takes days. Finding the next breakthrough cancer drug might still be like finding a needle in a haystack, but with AI, that’s no longer a time-intensive or daunting proposition.
In the Fast Forward landscape analysis of APNs, it’s an example of AI as a research assistant: AI to sort and analyze vast amounts of data to increase the capacity and speed of research.
Recommendations for Leveraging AI
Our research has generated a set of recommendations for nonprofits looking to apply AI in their own work on health care and equity.
- Enhance, don’t replace. Nonprofits should focus on AI-assisted technology to enhance human efforts rather than replace humans entirely. While AI technologies are advancing quickly, using AI to enhance the proven impact models and theories of change gives nonprofits the best chance at continuing to deliver impact and maintain a standard of quality in their work.
- Ethical and privacy considerations are paramount: Given the sensitive nature of healthcare data, nonprofits leveraging AI should prioritize ethical and privacy measures for safeguarding patient data, and take steps to limit algorithmic biases. Dhar advocates for building an internal culture “that prioritizes ethics, open communication, and continuous learning. Building this culture requires detailed, mandatory training on data collection and storage, norms around data use and ownership, and methods for auditing bias, privacy, and security.”
- Start with the problem, not the solution: AI tools might appear to have numerous applications in every area of a nonprofit's work and it’s certainly in vogue to say you’re using AI, but the APNs we studied identified not only specific use cases where AI could significantly enhance their work but also areas to avoid where AI was a solution looking for a problem.
- Start small, scale responsibly: Many of the healthcare APNs we studied were not afraid to launch early versions of their AI tools and refine them over time. But they paired early demos and pilots with substantial human oversight to make sure the AI was generating accurate results. Simple is smart. Complex systems require longer to get going and extensive ongoing maintenance. Simple AI tools enable small, local teams to learn by doing, all while keeping ongoing maintenance at a minimum.
- AI is only as good as the training data. Nonprofits should ensure their training data is substantial in size, diverse and representative, and clean. Jacaranda places a big emphasis on ensuring its training data is not only large enough to generate nuanced responses but also adjusted for the specific context in which the model is deployed (low-resourced contexts in Sub-Saharan Africa). For Jacaranda, which operates in three different languages, the training data must be language-sensitive to ensure responses come back in a language that the user can read and act on.
Whether it’s cancer drug researchers or frontline health workers in India, people working on the frontier of health care now have an indispensable partner: AI. But in each context, users need an expert-informed, patient-driven, and equity-focused plan to apply it responsibly.
AI has the power to change our understanding of the inherent tradeoffs between access to care, quality of care, and cost of care. As more and more nonprofits use AI, it will redefine our understanding of how health care can center the needs of communities everywhere.